Here’s the answer from Medica, to the letter in my previous post. The writer clearly spent a lot of time on her response, and she answered one of my questions, which is that my MRI would, or should, be covered. She also mentions my second question. That one is about the wrong doctor listed, as the person who ordered my PET scan. Unfortunately, solving that problem will take more of my time, for a mistake I didn’t make.
These questions and letters are amazingly dull and time consuming, but it’s the Corporate Health Care that so many are fighting so hard to keep.
Dear Mr. (Name Removed),
Thank you for contacting Medica regarding your out-of-network authorization letters.
I have attached the letters for your convenience and sent them via mail please allow 7-10 business days to receive them.
The authorization that we received for the PET Scan was submitted by Mansih Kohli MD. As long as Doctor Manish Kohli is the ordering physician on the claim it will pay as your in-network x-ray and imaging benefits. Please consult with your physician for additional information regarding the PET Scan. If your physician has any questions they may contact Medica Provider Services at 1-800-458-5512.
When you receive an eligible in-network PET Scan it is subject to your in-network $100 calendar year deductible, once satisfied you are covered 100% for the remaining of the calendar year.
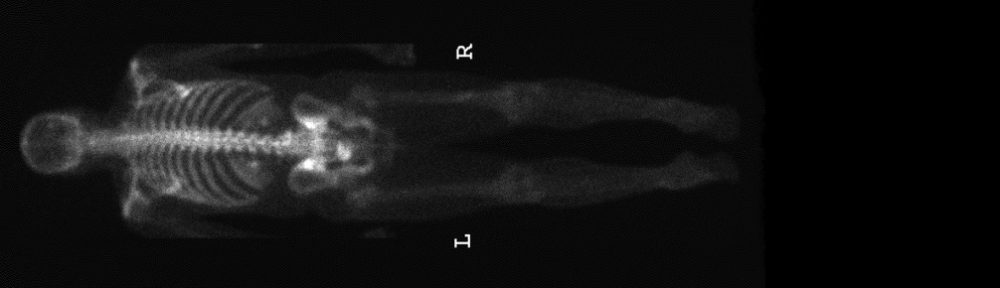
A Pelvic MRI needs to be doctor ordered (prescribed), it does not require a prior authorization. When you have an in-network MRI it is a $40 copayment per visit.
When you have services provided in an in-network facility it is subject to your in-network $100 calendar year deductible, once satisfied you are covered 100% for the remaining of the calendar year.
You have satisfied your in-network $100 calendar year deductible and $1,387.96 towards your combined in-network and out-of-network $2,500 calendar year maximum out-of-pocket. Your deductible and maximum out-of-pocket accumulations starts over January 1, 2018.
You may view the Summary of Benefits at www.umn.edu/ohr/benefits.
You can find additional information about your claims and benefits on mymedica.com:
• Choose Find a Doctor to find network providers.
• Click on View My Claims to review your claim information.
• Click on Account Balance to view your out-of-pocket amounts.
A final decision to pay or deny a claim will not be made until the claim is received. If you have additional services during your visit other benefits may apply.
I hope this information is helpful and I apologize for any frustration or inconvenience this may be causing you. If you wish to request reconsideration of your benefits, please reply to this email with a request for reconsideration. Please include in your email the outcome that you are requesting.
If you have any further questions, please contact Medica Customer Service at 1-877-252-5558 or go to www.medica.com/members and click on Contact us online.
Sincerely,
(Name Removed)
Consumer Advocate
Medica
Medica does not discriminate on the basis of race, color, national origin, sex, age, or disability in its health programs and activities. Read our policy.